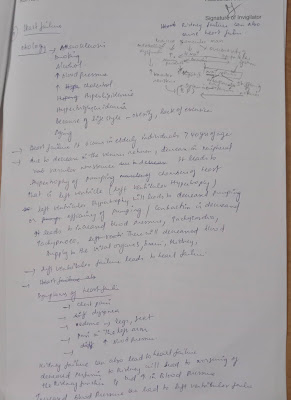
BDS 2nd internal assessment exam
1. Anatomical and etiologic localisation for harmiparesis and further management (9 marks)
Clinical Significance
Examination of the motor system of a limb includes checking for muscle bulk and fasciculation, muscle tone at joints, the power of muscle groups, deep tendon reflexes, clonus, plantar response, and coordination. In cases of a lower motor neuron type weakness, there is early muscle wasting, fasciculations, hypotonia, hyporeflexia, and a normal plantar response. On the other hand, the upper motor neuron type of weakness is characterized by normal muscle bulk, hypertonia, hyperreflexia, clonus, and an extensor plantar response (positive Babinski’s sign). Furthermore, the preservation of deep tendon reflexes distinguishes myopathy from neuropathy.
Lower motor neuron type weakness can result from any pathology of anterior horn cells, spinal nerve roots, plexus, or peripheral nerves. An upper motor neuron paraplegia can result from myelopathy involving the thoracic spinal cord, while cervical myelopathy would result in quadriplegia. The uppermost dermatomal level of accompanying sensory loss can further localize the lesion to the corresponding spinal segment. Myelopathy is further classified into compressive and non-compressive myelopathy. An example of non-compressive myelopathy is transverse myelitis that can be partial or complete. Compressive myelopathy can result from compression from the outside like a vertebral fracture, vertebral metastasis or subdural abscess or hematoma, or from the inside with conditions such as syringomyelia or hematomyelia.
Hemiplegia can result from a unilateral lesion of the brain stem, internal capsule, or cerebral cortex. Brain stem lesions result in crossed hemiplegia. For example, a left pontine lesion will result in left facial weakness of lower motor neuron type and right-sided hemiplegia. Similarly, a lesion in the left midbrain will result in left-sided oculomotor weakness with right hemiparesis and right facial weakness of upper motor neuron type. This constellation of signs is called Weber syndrome. Lesions above the level of the brainstem result in uncrossed hemiplegia. For example, a lesion in the left internal capsule would result in right hemiplegia and right facial weakness of the upper motor neuron type. A left cortical lesion may also result in cortical dysfunction in addition to right hemiparesis and facial weakness of upper motor neuron type.[5][6][7]
Link-https://www.statpearls.com/ArticleLibrary/viewarticle/40985
Link- https://www.spinalcord.com/blog/what-is-the-difference-between-hemiplegia-and-hemiparesis
2. Etiology pathogenesis clinical features management complications of acute pancreatitis

Symptoms
- A fat pad in the upper back or base of the neck (You may hear this called a "buffalo hump.")
- Thinning skin that is easy to bruise
- Acne
- Being very tired
- Weak muscles, especially when using your shoulders and hip muscles
- High blood pressure
- High blood sugar levels
- Depression and anxiety
- Osteoporosis
- Kidney stones
- Sleep problems
- Extra hair growth on your body and face
- Irregular periods
- Low sex drive and problems having an erection
- Decreased fertility
Etiology
All the factors which contribute to increased pressure in the left side and pooling of blood on the left side of the heart can cause cardiogenic pulmonary edema.[3] The result of all these conditions will be increased pressure on the left side of the heart: increased pulmonary venous pressure--> increased capillary pressure in lungs--> pulmonary edema.[4]
- Coronary artery disease with left ventricular failure (myocardial infarction)
- Congestive heart failure
- Cardiomyopathy
- Valvular heart diseases on the left side of the heart (stenosis and regurgitation)
- Cardiac arrhythmias
- Right to left shunts
- Increased pressure/pooling--> Increased pulmonary venous pressure--> Increased pulmonary capillary pressure--> fluid in interstitial spaces--> Increased pressure in Interstitial spaces--> fluid in alveoli (pulmonary edema).
- Link ,-https://www.ncbi.nlm.nih.gov/books/NBK544260/
There are two distinct phases of leptospiral infection in the body first, septicemic phase and second, immune phase.
The pathogenesis of leptospirosis is not fully understood. In the septicemic animal models, vascular injury is seen in various organs.16 Spirochetes can be found in the walls of capillaries and medium- and large sized vessels. The exact mechanism of vascular damage is not clear. A direct toxic effect of the leptospires has been proposed to cause the vascular injury, but no bacterial endotoxin has been demonstrated.
In the immune (second) phase of illness, the host immune response, including immune complex deposition, may play a role in endothelial injury.
During septicemic phase, invading leptospires are distributed throughout the body. Penetration and invasion of tissues is presumably accomplished through a burrowing motion produced by a pair of axial filaments and release of hyaluronidase.17 The dissemination and proliferation of spirochetes in various tissues results in a systemic illness, which has a broad spectrum of clinical manifestation. Generalised petechiae and ecchymosis occur in most internal organs in a severe case. Main organs affected are kidney, liver, brain and meninges. Microscopically, a systemic vasculitis with endothelial injury is seen. The damaged endothelial cells usually show different degrees of swelling, necrosis and denudation. The main histopathologic changes are usually found in the liver,18 kidney, heart and lungs. Hepatic lesions include mild degenerative changes in hepatocytes, prominent hypertrophy and hyperplasia of Kupfer cells, erythrophagocytosis and cholestasis. Focal necrosis with occasional acidophilic bodies may occur, but there is no particular zonal distribution associated with the necrosis. Mild to moderate mononuclear cell infiltrates are present in portal tracts. In the kidney, the main histopathologic feature is diffuse tubulointerstitial inflammation characterized by cellular infiltration with lymphocytes, plasma cells, macrophages and polymorphonuclear leucocytes. Tubular necrosis is also a common finding. Glomeruli show mild hyperplasia of mesangial cells and occasional infiltration with inflammatory cells. Grossly the lungs are heavy and severely congested, with focal areas of hemorrhage. Microscopically the lungs show congestion with foci of intraalveolar hemorrhage. In some cases pulmonary lesions include diffuse alveolar damage and variable degrees of airspace disorganization.
CLINICAL MANIFESTATIONS
In its mild form, leptospirosis may present as an influenza-like illness with headache and myalgia. Severe leptospirosis, characterized by jaundice, renal dysfunction, and hemorrhagic diathesis, is referred to as Weil's syndrome.
Incubation Period: 2-26 days (usually 7-12 days)
In general, clinical manifestation can be divided into two distinct clinical syndromes. 90% of patients present with mild anicteric febrile illness; 10% are severely ill with jaundice and other manifestations (Weil's disease). Both anicteric and icteric leptospirosis may follow a biphasic course (Table 1).19,20
Anicteric leptospirosis is the more common and milder form of the disease, and is often biphasic. In the first or septicemic phase, patients usually present with an abrupt onset of fever, chills, headache, myalgia, skin rash, nausea, vomiting, conjunctival suffusion, and prostration. Leptospires can be isolated from blood, cerebrospinal fluid (CSF), and tissues. The fever may be high and remittent reaching a peak of 40°C before defervescence. Conjunctival suffusion is characteristic and usually appears on the third or fourth day. Myalgias usually involve the muscles in the calf, abdomen, and paraspinal region and can be severe. When present in the neck, myalgias may cause nuchal rigidity reminiscent of meningitis. In the abdomen, myalgia may mimic acute abdomen, leading to confusion with surgical intra-abdominal emergencies. The skin manifestations seen in mild leptospirosis include transient urticarial, macular or maculopapular, erythematous or purpuric rash.21 The first phase lasts 3-9 days followed by 2-3 days of defervescence, after which the second or "immune" phase develops.
The immune phase, is characterized by leptospiruria and correlates with the appearance of IgM antibodies in the serum. Leptospira now settle in glomeruli and are eliminated from all sites in the host except eye and perhaps brain, where they may persist for weeks or months. Fever and earlier constitutional symptoms recur in some patients, and signs of meningitis, such as headache, photophobia, and nuchal rigidity may develop. Central nervous system (CNS) involvement in leptospirosis most commonly occurs as aseptic meningitis. Complications such as optic neuritis, uveitis, iridocyclitis, chorioretinitis, and peripheral neuropathy occur more frequently in the immune phase. Prolonged or recurrent uveitis was demonstrated in 2% of patients with onset several months after symptoms of clinical leptospirosis. 22 A rare but severe manifestation is hemorrhagic pneumonia. The illness in anicteric leptospirosis may be self-limited, lasting 4-30 days, with complete recovery as a rule.
In icteric leptospirosis (Weil's syndrome) (usually caused by L. icterohaemorrhagiae), persistent high fever and jaundice may obscure the two phases. This is usually associated with hepatic dysfunction, renal insufficiency, hemorrhage and multi-organ failure (MOF). Hemorrhage can occur as petechiae, purpura, conjunctival hemorrhage and gastrointestinal hemorrhage. MOF is associated with a very high mortality. Myocarditis and hemorrhagic pulmonary infiltration are other complications, which may prove fatal.
Causes
Heart failure often develops after other conditions have damaged or weakened the heart. However, heart failure can also occur if the heart becomes too stiff.
In heart failure, the main pumping chambers of the heart (the ventricles) may become stiff and not fill properly between beats. In some people, the heart muscle may become damaged and weakened. The ventricles may stretch to the point that the heart can't pump enough blood through the body.
Over time, the heart can no longer keep up with the typical demands placed on it to pump blood to the rest of the body.
Your doctor can determine how well your heart is pumping by measuring how much blood is pumped out with each beat (ejection fraction). Ejection fraction is used to help classify heart failure and guide treatment. In a healthy heart, the ejection fraction is 50% or higher — meaning that more than half of the blood that fills the ventricle is pumped out with each beat.
But heart failure can occur even with a normal ejection fraction. This happens if the heart muscle becomes stiff from conditions such as high blood pressure.
Heart failure can involve the left side (left ventricle), right side (right ventricle) or both sides of your heart. Generally, heart failure begins with the left side, specifically the left ventricle — your heart's main pumping chamber.
| Type of heart failure | Description |
|---|---|
| Left-sided heart failure | Fluid may back up in the lungs, causing shortness of breath. |
| Right-sided heart failure | Fluid may back up into the abdomen, legs and feet, causing swelling. |
| Systolic heart failure (also called heart failure with reduced ejection fraction) | The left ventricle can't contract vigorously, indicating a pumping problem. |
| Heart failure with preserved ejection fraction | The left ventricle can't relax or fill fully, indicating a filling problem link-https://www.mayoclinic.org/diseases-conditions/heart-failure/symptoms-causes/syc-20373142. |
Box 1: Red flag conditions indicating possible underlying spinal pathology or nerve root problemsw9
Red flags
Onset age < 20 or > 55 years
Non-mechanical pain (unrelated to time or activity)
Thoracic pain
Previous history of carcinoma, steroids, HIV
Feeling unwell
Weight loss
Widespread neurological symptoms
Structural spinal deformity
Indicators for nerve root problems
Unilateral leg pain > low back pain
Radiates to foot or toes
Numbness and paraesthesia in same distribution
Straight leg raising test induces more leg pain
Localised neurology (limited to one nerve root


























Comments
Post a Comment